Glaucoma
Glaucoma is a poorly understood group of diseases that damage the optic nerve, resulting in permanent vision loss and blindness, if not properly treated. Glaucoma, a leading cause of blindness and visual impairment, can affect patients of all ages but is more common in older adults. Glaucoma is the number one preventable cause of blindness in the world. Many people affected by glaucoma do not experience any symptoms and may not be aware that they have the disease until they have lost a significant amount of vision. With early detection and treatment, however, eyes can be protected against the serious loss of vision or blindness. Catching glaucoma at an early, treatable stage is one important reason to have thorough eye examinations regularly.
Risk Factors for Glaucoma
There are several factors that increase the risk of developing glaucoma, including:
Age - the older you are, the more at risk
Having a family history of glaucoma
Having elevated intraocular pressure
Having a history of a major eye injury or trauma
Having certain medical conditions, like diabetes
Prolonged use of oral or topical corticosteroids (ie. prednisone)
Patients with risk factors for the disorder should be especially vigilant about having regular eye examinations.
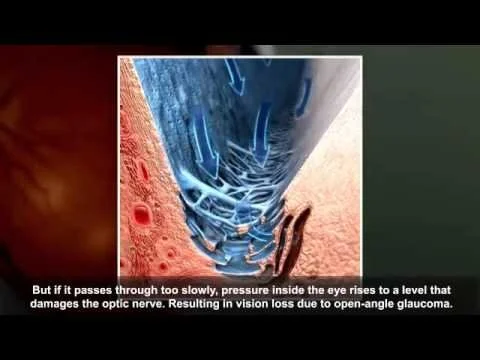
Causes of Glaucoma
Certain diseases or conditions can contribute to the development of glaucoma. These include:
Increased pressure within the eye
Severe eye infection or inflammation
Injury to the eye
Blocked blood vessels
Types of Glaucoma
There are several types of glaucoma. The two most common types are Primary Open Angle Glaucoma (POAG), and Narrow Angle (NAG) or Angle Closure Glaucoma (ACG). Narrow anatomical angles can lead to angle-closure which can acutely increase the pressure in the eye causing damage to the optic nerve. Childhood glaucoma may start in infancy, childhood, and adolescence. Other types of glaucoma, which occur much more rarely, include:
Low Tension Glaucoma
Congenital Glaucoma
Secondary Glaucoma
Pigmentary Glaucoma
Pseudoexfoliation Glaucoma
The vast majority of glaucoma cases are open angle, and very slow progressive conditions. There is plenty of time to monitor and adjust effective treatment. A minority of cases are narrow angle, which can lead to closed angle glaucoma. If narrow angles progress to angle closure, this issue becomes quickly urgent, and must be treated on an urgent basis. Most narrow angle cases should be treated with a laser with a procedure called Laser Peripheral Iridotomy (LPI) to prevent the progression to angle closure. A closed angle in an eye is considered an emergency, and should be treated immediately with LPI.
Symptoms of Glaucoma
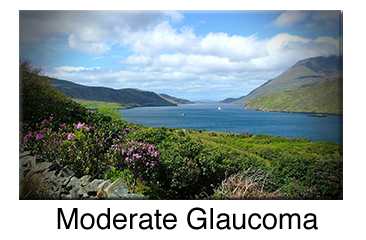
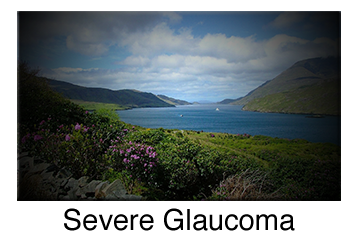
It is important to remember that patients with early, mild or moderate stage glaucoma will not have any symptoms. There is no pain, no blur, no obvious loss of vision. By the time symptoms occur, the disease is advanced and much more difficult to arrest. At this point, eye surgery is usually necessary to prevent total blindness.
There are usually no warning signs or symptoms of Open-Angle Glaucoma. The disease usually progresses to gradual loss of peripheral vision in the mild to moderate stages, then degrades to tunnel vision in advanced cases. If not effectively treated at this point, total blindness will occur.
The symptoms of angle-closure glaucoma due to a sudden increase in intraocular pressure from the closure of drainage canals may include:
Eye pain
Nausea and vomiting
Blurred vision
Halos around lights
Red eyes
Headache
How Glaucoma Can Affect Your Vision
Diagnosis of Glaucoma
The diagnosis of glaucoma is made after a comprehensive medical examination of the eye and a review of the patient's medical history. Specific diagnostic tests are necessary to confirm the diagnosis. Testing may include some of the following:
Tonometry
Tonometry measures the pressure within your eye. During tonometry, eye drops are used to numb the eye. Then a doctor or technician uses a device called a tonometer to measure the inner pressure of the eye. The range for normal pressure is 08-23 mmHg (“mmHg'' refers to millimeters of mercury, a scale used to record eye pressure). Most glaucoma cases are diagnosed with pressure exceeding 20 mm Hg. However, some people can have glaucoma at pressures between 12 -22mm Hg. Eye pressure is unique to each person.
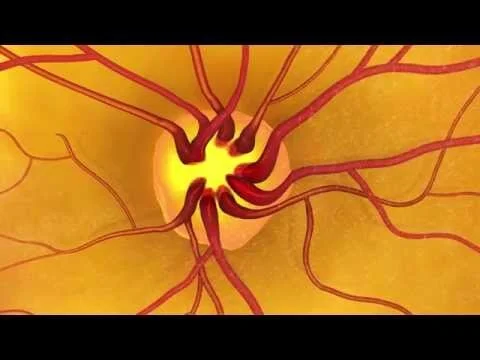
Ophthalmoscopy
This diagnostic procedure helps the doctor examine your optic nerve for glaucoma damage. Eye drops are used to dilate the pupil so that the doctor can see through your eye to examine the shape and color of the optic nerve. The doctor will then use a small device with a light on the end to light and magnify the optic nerve. If your intraocular pressure (IOP) is not within the normal range or if the optic nerve looks unusual, Dr. Massengale will recommend that you undergo a battery of tests needed to ascertain the presence and degree of damage. This tests are routinely repeated in order to monitor progression of the disease.
Perimetry (Visual Field Testing)
Perimetry is a visual field test that produces a map of your complete field of vision. This test will help determine whether your vision has been affected by glaucoma. During this test, you will be asked to look straight ahead as a light spot is repeatedly presented in different areas of your peripheral vision. This helps draw a "map" of your vision. Do not be concerned if there is a delay in seeing the light as it moves in or around your blind spot. This is perfectly normal and does not necessarily mean that your field of vision is damaged. Try to relax and respond as accurately as possible during the test. After glaucoma has been diagnosed, visual field tests are usually done one to two times a year to monitor any changes.
Gonioscopy
This diagnostic exam helps determine whether the angle where the iris meets the cornea is open, narrow or closed. During the exam, eye drops are used to numb the eye. A hand-held gonioscopy lens is gently placed on the eye. This contact lens has a mirror that shows if the angle between the iris and cornea is closed and blocked (a possible sign of angle-closure or acute glaucoma) or wide and open (a possible sign of open-angle, chronic glaucoma).
Pachymetry
Pachymetry is a simple, painless test to measure the thickness of your cornea —the clear window at the front of the eye. A probe called a pachymeter is gently placed on the front of the eye (the cornea) to measure its thickness. Pachymetry can help your diagnosis because corneal thickness has the potential to influence eye pressure readings. With this measurement, Dr. Massengale can better understand your pressure (IOP) reading and develop a treatment plan that is right for you. The procedure takes only about a minute to measure both eyes.
Once glaucoma has been diagnosed, treatment should begin as soon as possible to help minimize the risk of permanent vision loss.
Treatment of Glaucoma
There is no cure for glaucoma, so treatment focuses on preventing progression. Some of the treatment methods for glaucoma are as follows:
Pressure lowering eye drops
Laser Procedures (SLT, LPI)
Oral Medications
Laser Surgery
The type of laser surgery will depend on the form of glaucoma and how severe it is. Lasers produce a focused beam of light that can make a very small opening in your eye tissue, depending on the strength of the light beam. Laser surgeries are performed in an outpatient setting. During the laser surgery, the eye is numbed so that there is little or no pain. Your eye doctor then holds a special lens to the eye. The laser beam is aimed into the eye, and there is a bright light, like a camera flash.
The following are the most common laser surgeries to treat glaucoma.
Selective Laser Trabeculoplasty (SLT)
For the treatment of primary open-angle glaucoma (POAG).
SLT uses a laser that works at very low levels. It treats specific cells "selectively,” leaving untreated portions of the trabecular meshwork intact. For this reason, SLT may be safely repeated.
SLT may be an alternative for those who have been treated unsuccessfully with ALT or pressure-lowering drops.
Argon Laser Trabeculoplasty (ALT)
For the treatment of primary open-angle glaucoma (POAG).
The laser beam opens the fluid channels of the eye, helping the drainage system work better. In many cases, medication will still be needed.
Usually, half the fluid channels are treated first. If necessary, the other fluid channels can be treated in a separate session another time. This method prevents over-correction and lowers the risk of increased pressure following surgery. Argon laser trabeculoplasty has successfully lowered eye pressure in up to 75% of patients treated.
Laser Peripheral Iridotomy (LPI)
For the treatment of narrow angles and narrow angle or angle closure glaucoma.
Narrow angles, NAG and ACG occur when the angle between the iris and the cornea in the eye is too small. This causes the iris to block fluid drainage, increasing inner eye pressure. LPI makes a small opening in the iris, allowing it to fall back from the fluid channel and helping the fluid drain.
Side effects from Glaucoma Laser Surgery
There is a slight stinging sensation associated with LPI and ALT
Long-term Benefits of Glaucoma Laser Surgery
Glaucoma laser surgeries help to lower the intraocular pressure (IOP) in the eye. The length of time the IOP remains lower depends on the type of laser surgery, the type of glaucoma, age, race, and many other factors. Some people may need the surgery repeated to better control the pressure IOP.
Medication Following Laser Surgery
In most cases, medications are still necessary to control and maintain eye pressure. However, surgery may lessen the amount of medication needed.
Recovery Time
In general, patients can resume normal daily activities the next day after laser surgery. Before the surgery, your eye will be numbed with medicine. Your eye may be a bit irritated and your vision slightly blurry after the surgery. You should arrange a ride home after your surgery.
Risks of Laser Surgery
As with any type of surgery, laser surgery can carry some risks. Some people experience a short-term increase in their intraocular pressure (IOP) soon after surgery. The use of anti-glaucoma medication before and after surgery can help to reduce this risk. There is also a small risk of intraocular bleeding from the procedure. It is generally resolved within a few seconds by Dr. Massengale applying pressure to the eye with the laser lens, allowing the normal coagulation process to the damaged blood vessels in the iris.
Increased Risk of Cataracts
There is a small risk of developing cataracts after some types of laser surgery for glaucoma. However, the potential benefits of the surgery usually outweigh any risks. There is a common myth that lasers can be used to remove cataracts; this is not the case except in experimental studies.
It is important to discuss all of your questions or concerns about laser surgery with your eye doctor.